|
What Is Urogynecology?

Urogynecology is a subspecialty within Obstetrics and Gynecology dedicated
to the treatment of women with pelvic floor disorders such as urinary incontinence (leakage of urine) and prolapse (falling)
of the vagina, bladder and/or the uterus.
How Common Is Urinary Incontinence Among Women?
Many women incorrectly assume that urine leakage is normal. While the problem of
urine leakage is very common, it should never be considered normal. Urinary incontinence is a very common condition affecting
at least 10-20% of women under age 65 and up to 56% of women over the age of 65. While incontinence also affects men it occurs
much more commonly in women.
What Causes Urinary Incontinence?
- Urinary incontinence is a symptom, not a disease and there are many
possible causes. A women with incontinence will be referred to a gynecologist by her health care provider for further
consultation. The key to treatment is identifying the specific type(s) of incontinence that a woman has through a careful
medical interview and focused physical exam. The two most common types of urinary incontinence are stress incontinence and
urge incontinence.
Stress incontinence is urine leakage that happens during activity that causes pressure on the bladder
such as laughing, lifting, coughing or sneezing.
Urge incontinence is urine leakage that occurs before a woman has
a chance to get to the bathroom in response to an urge to urinate. Women with this type of leakage may also experience frequent
urges to urinate and frequent nighttime waking to urinate.
What Treatment Options Are Available?
Stress incontinence can be effectively treated with pelvic floor
exercises, devices that "block" the loss of urine, or surgery. There is also a new medication called Duloxetine that will
soon be available for the treatment of stress incontinence. Urge incontinence is commonly treated with medications, biofeedback,
or electrical stimulation to the nerves that control the bladder. There is even a new treatment for urge incontinence that
involves placement of an electrical stimulator under the skin (similar to a pacemaker). The most important thing to remember
is that there is a wide variety of non-surgical and surgical treatment options available for all kinds of urinary incontinence.
Overactive Bladder
What Is An Overactive Bladder?
An overactive bladder is a condition that results from sudden, involuntary
contraction of the muscle in the wall of the urinary bladder. Overactive bladder causes a sudden and unstoppable need to urinate
(urinary urgency). Overactive bladder is also referred to as urge incontinence and is a form of urinary incontinence (unintentional
loss of urine),
What Are The Symptoms Of Overactive Bladder?
Overactive bladder symptoms may mean you:
- Feel a strong, sudden urge to urinate
- Experience urge incontinence, the unintended loss of urine immediately following
an urgent need to urinate
- Urinate frequently, usually eight or more times in 24 hours
- Awaken two or more times in the night to urinate (nocturia)
What Are The Causes Of Overactive Bladder?
The symptoms of
overactive bladder occur in most cases because the muscles of the bladder involuntarily contract when it's still filling and
only about half full. This contraction creates the urgent need to urinate. The urinary sphincter may remain constricted and
prevent the bladder from emptying. If not, then a person experiences urge incontinence.
In many cases doctors can't exactly identify overactive bladder causes. Several
factors may cause or contribute to symptoms similar to those of overactive bladder and your gynecologist will try to
rule out these during an evaluation because these require other specialized treatments. These include:
- Urinary tract infection
- Inflammation of tissues near the urinary tract
- Abnormalities in the bladder, such as tumors
- Factors that obstruct bladder outflow (enlarged prostate, constipation, bladder
stones)
- Diabetes, which can cause excess urine production
- Excess consumption of caffeine or alcohol
- Medications that cause a rapid increase in urine production
What Are Treatment Options For Overactive Bladder?
Your gynecologist is likely to recommend a combination of overactive bladder
treatment strategies to alleviate your symptoms.
Behavioral Interventions
Behavioral interventions can help you manage overactive bladder. If you experience
urge incontinence, these interventions alone aren't likely to result in complete dryness, but they will reduce the number
of incontinence episodes. The interventions your doctor will recommend may cover the following areas:
- Fiber intake
- Bladder training
- Double voiding
- Scheduled toilet trips
- Pelvic floor muscle exercises
- Absorbent pads
Medications
Clinical trial evidence shows that medications called anticholinergics
are the most effective for alleviating symptoms of overactive bladder and reducing episodes of urge incontinence. These drugs
include Detrol, Ditropan, Oxytrol, Sanctura and Vesicare.
Surgery
Surgery to treat overactive bladder is reserved for people with severe cases who don't respond
to other treatments. The goal is to improve the bladder's storing ability and reduce pressure in the bladder.

Prolapse
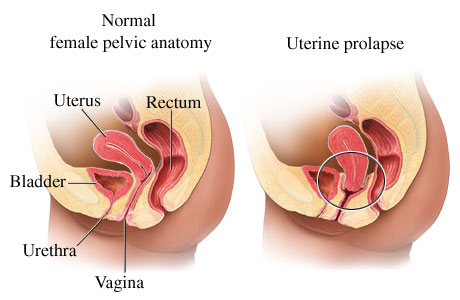
What Does Prolapse Mean?
The word prolapse simply means displacement from the normal position.
When this word is used to describe the female organs, it usually means bulging, sagging or falling. It can occur quickly but
usually happens over the course of many years. There are various types of prolapse which can occur individually or together.
- What Are The Symptoms Of Prolapse?
-
The symptoms depend on which type of prolapse you have. Since
prolapse usually occurs slowly over time the symptoms can be hard to recognize. Most women don't seek treatment until they
actually feel something protruding outside of their vagina. The very first signs can be subtle such as pain during intercourse
or an inability to keep a tampon inside the vagina. As the prolapse gets worse, some women complain of a bulging or heavy
sensation in the vagina that worsens by the end of the day or during bowel movements.
- What Causes Prolapse?
-
There are many factors that seem to contribute to the development
of prolapse. Genetics, chronic coughing, vaginal deliveries, obesity, pelvic tumors and chronic constipation. Repetitive heavy
lifting may also contribute to prolapse.
- What Are Treatment Options For Prolapse?
-
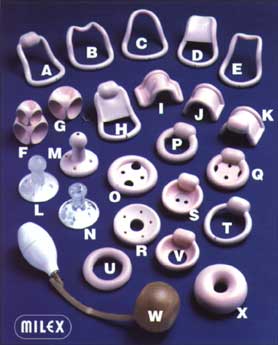
A pessary is the easiest, safest and quickest solution
outside of surgery of treating prolapse. A pessary is worn in the vagina like a diaphragm. Pessaries come in many different
shapes and sizes all designed to support the prolapsed pelvic organs.
- The ideal way to use a pessary is to insert it each day as part of
your morning routine and take it out for cleaning each night. When this is not possible, women come to a gynecologists office
about four to six times a year for an exam and pessary cleaning. Even when a pessary is worn almost continuously, vaginal
infections are rare.
How Will Prolapse Treatment Affect My Sex Life?
If you choose to use a pessary, your sex life shouldn't change, except
for the fact that the pessary usually needs to be removed prior to intercourse. If you have reconstructive surgery to correct
prolapse, it is recommended that you refrain from intercourse for three months after your operation to allow proper
healing. After waiting three months, getting used to having intercourse will take some time but most patients report an improved
sex life afterwards.
|
